

*日本語の記事はこちら
hosted by Cyber Civilization Research Center (CCRC), Keio University
co-hosted by the Medical Inclusion working group, CCRC
Life Intelligence System Consortium, SFC Research Institute
Value Society Platform Laboratory, SFC Research Institute
WIDE Project
Event Information
Date: Monday, July 4, 2022, 13:00-18:10 (Event reception opens at 12:30)
Place: G-lab, 6F, East Building, Mita Campus, Keio University
Click here to view the program
↓Seminar video first half: from the organizer’s greeting to before the panel discussion
↓Seminar video second half: from the panel discussion to the closing remarks
Organizers’ Greetings
Jun Murai, Professor and Co-Director, Cyber Civilization Research Center, Keio University

Medical and Health Care to Lead DX (Digital Transformation)
I’ve been working on providing a digital technology platform that will be useful to society in the long term. It is not difficult to put the technology in place, but it is challenging to do it in a way that is truly helpful: society needs not only to understand what it can do for us it but also be ready to use it.
With the crises of COVID-19 and the war in Ukraine, everyone has begun to appreciate the role of digital technology, i.e., how effective it can be even though not always helpful in all places.
We’ve been arguing for a long time about what kind of world we can create where everyone can use the internet. Now the world is in fact connected to the internet, and everyone is already using digital technology. The time has come for the application of the internet to societies as a whole; we can no longer make excuses.
We must form an environment where medical and health care are leading DX. This is why we have gathered here on behalf of the Japanese society. We can create such an environment and offer a new medical care system to the world at large.
Participant groups based at Keio University have supported the discussion in this context, and each group is represented here today. The purpose of this seminar is to integrate these groups and coordinate our knowledge. I hope that more diverse networks will be formed from here on.
Greetings from Keio University
Professor Masayuki Amagai, Vice President of Keio University

DX in the Medical Field Is not Straightforward
Digital transformation in the medical field is not a straightforward issue.
During my previous job as the director of the School of Medicine, Keio Hospital introduced electronic medical records. Initially, medical records were managed separately by each department in the hospital. The long road to launching consolidated electronic medical records in the hospital began with the transformation of multiple medical records per patient into a single record. Clearly, sharing medical records across departments in Keio University Hospital from 2012 was a huge step forward.
With AI hospital projects, connecting medical information has become more urgent than ever. In fact, medical data has been connected to various areas of health care in daily life and is about to create substantial new value.
Various issues and problems arise when connecting information, and this is why people with diverse backgrounds and with the ability to resolve such tricky issues are gathered here. I hope everyone here will become a leader in the field of medical DX.
Opening Remarks: Medical DX in the Near Future
Professor Sumio Matsumoto, Director Emeritus,
National Hospital Organization, Tokyo Medical Center

Despite Obstacles, Telemedicine Will Grow
Since 2015 I have been promoting ‘Hospital at Home,’ i.e., a telemedicine system using TVs in the patients’ homes connected to the medical network. At that time, smartphones and SNS had become widespread in Japan, especially among young people. I thought what people could do online would also work in the medical field because I realized that the question why medical care was not undertaken online was posed by the very people in need of it. In recent years, smartphones have rapidly become widespread among the elderly, so we must consider telemedicine through smartphones and TVs.
During the pandemic of COVID-19, the administration of Prime Minister Suga decided to lift part of the ban on telemedicine. However, patients have in fact died of acute exacerbation while waiting for help at home.
Is it possible to revitalize and expand digital technology in medical care? Yes indeed, we have a lot of scope with digital power in that area, namely:
- solving disparities in medical resources
- reforming the process of doctors’ task shifting
- accelerating telemedicine
- standardizing PHR (Personal Health Record) for each person
- providing e-learning for doctors
- constructing medical tourism
- producing new drugs such as vaccines made in Japan
However, innovation in these kinds of medical areas has been insufficient.
The operational schedule of the digital health reform process at the Ministry of Health, Labor and Welfare includes multiple functions related to PHR and reform of electronic medical records based on the HL7 FHIR. Although I am advisor to that process, I believe it is doubtful that it will actually be followed. Nevertheless, telemedicine has much potential in becoming widespread.
Today, I expect discussions of these problems, which occur due to vertically divided governance in the medical field. For example, emergency staff cannot smoothly coordinate arrangements with hospital staff via a patient’s Apple Watch due to the disconnect between the Fire and Disaster Management Agency in the Ministry of Internal Affairs, on the one hand, and hospitals under the Ministry of Health, Labor and Welfare, on the other.
Why Healthcare Data Sharing Does not Progress
-Learn From the Past and Think About the Near Future-
Motohiro Asonuma, Visiting Professor, Juntendo University,
Member of the Working Group on Cabinet Office National Strategic Special Zones

Strong Policy Guidance Is Needed to Share Medical Information
I have been involved in introducing medical information systems for about 50 years. As a result, I have experienced the difficulties faced by both system providers and parties striving for system implementation. I am aware of my responsibility in this area, especially regarding information sharing between medical facilities and regions.
There still exists the idea that medical information is the property of medical intelligence. The perception that medical records might also belong to patients has only become common over the last ten years. Unfortunately, the perception that they are also useful for others and for public health is still weak.
Although discussions about standardization were held in Japan, its implementation has been delayed. And information sharing hasn’t progressed at all due to many hurdles regarding privacy, thrown up by organizations and private entities, etc. There is no standard specification for introducing electronic medical records. As a result, separate, individually-based specifications remain in use everywhere.
Initially, the Japanese medical information system was in a leading position around the world. Unfortunately, although it has progressed over the years, improvements remain a patchwork which is unable to solve fundamental problems. In recent years, HL7 FHIR had been proposed so get medical information sharing back on track, but I could not agree with its formulation. Ten years ago, it was thought that medical information could be shared with SS-MIX. However, even though many discussions were held and social implementations repeatedly put forward, many troubling issues became apparent. It is therefore necessary to have concrete deliberations on how to proceed with DX based on HL7 FHIR.
Medical facilities and vendors have pursued localized optimization inside medical institutions and regions. The current situation where many proprietary protocol specifications are scattered about is not just a problem for vendors but also for government and the medical field. What we need are discussions aimed at the overall cross-sectional optimization of medical information and government policy.
Various barriers interfere with the sharing and utilization of medical information. It may be necessary to have pretty strong policy guidance. As you know, in Estonia, the Medical Service Organization Law requires medical institutions to provide medical information to the government, and standard protocols are in place for each type of information. I think Japan must make it mandatory to build data-sharing infrastructure along similar lines.
In the future, it will be necessary to smoothly share data of medical institutions, including health information and administrative information related to a wide range of individuals. Then, we must acquire the mindset that the operation of such a system allows ‘Data Exchange’ to build efficient data structures depending on the situation of the information provider. That is, there will be no need to justify only standardized specifications.
In addition, it will be essential to discuss the combination of demonstration experiments and unity across ministries and agencies. In the Working Group on Cabinet Office National Strategic Special Zones specialized in health, I will use my experience to contribute to issues such as data sharing, standardization and conducting demonstration experiments.
Challenges to Digital Services in Medical Information Systems
Nobuyuki Kobayashi, Director, Medical Information System Division,
Fujita Medical University Hospital

Fujita Health University Moving Ahead
In 2020, Fujita Health University accepted 128 passengers and crew members of the Diamond Princess because we thought one of the university’s missions was to support our country on the verge of a national crisis. Even now, under the same vision of ‘Fujita Health University moving ahead,’ we are working to improve smart hospitals and medical DX.
Our hospital has the highest number of beds in Japan and we are also in charge of the most comprehensive store of hospital-based medical information in Japan. As a result, we believe a medical information DX strategy is indispensable, and we are promoting a wide range of reforms throughout the university, including governance.
In smart hospitals, data browsing and connectivity inside and outside the hospital are crucial, and the re-evaluation of security is imperative. Therefore, I created a four-area model that classifies the fundamental categories of the medical information system as follows :
- general services
- the external system
- the hospital information utilization system
- the hospital business system
Each area is set up with its own security requirements and enabled with the mutual security
verification of out-of-hospital and in-hospital networks.
At Fujita Health University remote and robotic surgery projects have already been carried out ahead of others. In order to expand the range of remote surgery and diagnosis, wideband, low latency, and highly reliable networks are required. With these requirements in mind, we are planning an advanced medical information network specializing in medical care.
There is also a plan to build a standardized screening system based on FHIR and establish a PHR platform. Furthermore, we are working with medical IT venture companies to improve the efficiency of emergency medical care and introduce AI-based interviews.
We will continue to promote smart hospitals in the spirit of the vision of ‘Fujita Health University moving ahead.’
Teppei Sakano, Representative Director and CEO, Allm Inc.

‘Get With It’ Corona Model
The medical IT market is a rapidly accelerating new growth industry. Deregulation and industrial promotions are taking place worldwide due to COVID-19, but even in this situation Japan can still be a winner. Even though medical information is not extensively linked, every person’s medical and healthcare data life-time data has been collected in this country since WW2. This situation constitutes a rare business opportunity, so we have been reorienting our business in line with the ‘get with it’ corona model.
The DtoD (doctor-to-doctor) telemedicine app, ‘Join,’ which we developed in 2014, provides an environment where you can access medical information from a smartphone via video calls, text chats, and electronic medical records. In 2016, Join became Japan’s first medical device program covered by public insurance. We are already expanding globally and trying to become the platformer.
Initially, the app aimed to establish in-hospital communication between doctors across internal departments. However, it subsequently began to be utilized regionally for the cooperative provision of medical information, expanding to nationwide cooperation and international support, and covering more than 1100 facilities in 30 countries. In addition, during the COVID-19 pandemic, the app supported telemedicine by providing a free teaching file collection for infectious diseases.
With government support, we promote medical exports and worldwide medical aid through the ‘get with it’ corona model. By connecting universities in Japan and abroad, we are creating a global education program for medical DX, including distance education in surgery. We are also progressing collaborations with overseas medical IoT and AI venture companies which, by combining low-cost diagnostic tools with AI screening and telemedicine, allow companies to reduce cost.
Using our app, ‘MySOS,’ the PHR system under the ‘get with it’ corona strategy can support future infectious countermeasures. MySOS records physical indicators such as blood pressure and body temperature on a daily basis. It also analyzes data, including vaccine history and PCR test results. We are also developing a system that uses the latest AI, such as in identity and location information verification when entering Japan. We will continue to create businesses in response to surrounding circumstances, including measures fighting infectious diseases.
Seigo Hara, CEO and MD, MICIN Inc.

New Value of Online Medical Care
We envision ‘all people to live out their lives with dignity.’ With that motto, we are advancing telehealth, digital therapeutics, and insurance areas. Uniquely, we offer insurance for the sick, which integrates well with the digitization of medical care. In addition, we have created a system to provide telemedicine via TV to as many people who do not have a smartphone as possible.
The system of telemedicine has changed significantly over the last few years. Restrictions on telemedicine were partly lifted in 2015 but were not functional. However, since 2020, the government has eased restrictions on telemedicine in view of the COVID-19 pandemic. And this year, some temporary measures have been made into permanent ones. Since the onset of the pandemic, our services, including the telepharmacy service, have recorded over 10,000 cases.
During the COVID-19 crisis, there was an urgent need for contactless medical treatment for as many patients as possible. Therefore, we developed an app, ‘Curon TypeC,’ that matches doctors to patients in a virtual waiting room. It provides more extensive access to medical care for patients waiting at home while optimizing medical resources and reducing the workload of health centers. This example goes beyond the framework of one-on-one medical care and throws some light on the potentially new value of online medical care.
Although there are a number of hurdles, I believe that with online digital services we can provide better value-added medical care and utilize datasets with greater accuracy than is possible face-to-face.
Telemedicine will become the gateway to access medical care and digital health and medical information.
Reiji Oishi, Representative Director and CEO, Healthcare Technologies Corp.

Connect Medicine With Daily Life Through Digital Technologies
Healthcare Technologies Corp. was established as a subsidiary of Softbank to solve social issues in the medical field through digitization.
For the next generation, a world where people would be able to live healthier lives, we released ‘Helpo’ in 2020. Its purpose is to bring about a society where everyone can be naturally healthy and prolong their lives. On the app we enabled health and medical consultations 24 hours a day, 365 days a year, with follow-up support for infected patients. Doing so we could reduce the work overload of local governments during the COVID-19 crisis.
‘Helpo’ is a daily-use application that is envisaged to summarize patient life data and connect with efficient medical care through its gateway. Digital and medical care are essential life infrastructures that must be joined seamlessly. We will continue to create a useful medical platform using digital means.
Naohisa Yahagi, M.D., Ph.D.,
Professor at Graduate School of Media and Governance, Keio University,
Head of Digital Health, Digital Agency
Co-Creating Medical Care as Social Infrastructure
The medical system in Japan is excellent, so I want to integrate it with our social infrastructure for future generations. The clinical application of technological innovations such as digital technology refines medical care as a social system, sophisticating and streamlining the medical field.
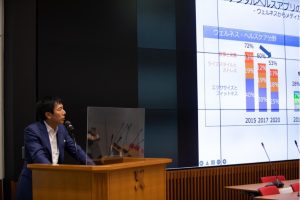
Medical DX is a global trend, and the number of digital health applications has increased dramatically. Furthermore, research on the effectiveness of applications has also increased in recent years. Highly mature applications have been developed since around 2017, and these applications tend to manage patient status and provide medical navigation systems.
In Japan, there is little structured data that can be used for high-quality analysis of medical care. However, it is necessary to focus on a mechanism that utilizes and associates individual medical and health care data because the overwhelming majority of patients would like to see their medical data used if it is helpful to someone.
Medical care is social infrastructure. Thus, government, people, and medical staff must collaborate in co-creative innovation to build world-leading technologies and new medical services. Assembling a team and producing a grand design from multiple viewpoints is necessary to convert a functionally limited machine-centered system into a system that sees people at its middle.
Tomohiro Sonoo, CEO, TXP Medical Inc.

Connection of Medical Information
At a front-line position of emergency medical DX, we aim to solve problems arising in the medical information division. However, much data inside hospitals is still disconnected. And data related to ambulance crews, municipal arrangements and individual hospitals is also not connected. Since the establishment of our company, we have been promoting DX for work in hospital emergency departments, which used to be managed with paper. Our service has received high approval from many university hospitals and is set to establish a position as a platformer in the emergency department.
In addition, we have been promoting DX for regional ambulance transportation. We want to solve the problems of emergency transportation by improving the efficiency of bucket brigade information in areas where digital technology has not been utilized. In the first instance, using AI, we want to develop an OCR-based information input support system. This would enable emergency services to input patient information as quickly as it is written down by hand.
It is crucial to produce a system that will have a future in the medical field. Therefore, we promote DX in conjunction with many others involved in consulting.
Panel Discussion
“The Present and Future of Medical DX

(Murai)
What kind of expertise has the capacity to advance medical DX? I think one role of universities is to produce the required human resources. In fact, I was in charge of personnel with a view to have Dr. Yahagi join Keio’s Faculty of Environment and Information. I also thought it was important for medical personnel to collaborate with other fields in the interdisciplinary area. Mr. Sakano seems to be working with visionary sweep, so what do you think is the key to the allocation of human resources?
(Sakano)
In the field of medical DX, many people have a similar background in brilliant careers such as those of doctors, and are highly educated. But I have no medical experience at all. I come from the IT area, so there was a need for me to accept the opinion of people in the medical field. The same is true when handling regional medical information and forming links between hospitals, where we must make budget adjustments and consider the position of all those involved in collaboration with local governments. So, not only doctors but also local governments, the national government, academic societies, and other stakeholders join the project. Cooperation is greatly needed, but creating a collaborative system happens to suit the characteristics of Japanese people. Therefore, smart-city projects that need to consider the mechanism of urban development and what to do with the surrounding region should be very marketable overseas.
:
(Murai)
Some people have said that Japanese medical care is excellent, but what is Japan’s position in relation to the world, and what kind of contribution can it make through medical DX?
(Yamamoto)
Japan is experiencing the characteristics of an aging society, but we have the ability to lead in the area of health. The Japanese have an advanced culture and are likely to find solutions to problems in medical and healthcare policy while also ensuring personal freedom. This point would receive world attention.
(Oishi)
Vision Fund has funded very few Japanese companies. No single company leads in AI and DX, so our country must find ways to support the growth of this market. Japan is very aware of the need to promote medical and health care, and I expect Japanese companies to grow accordingly.
(Hara)
I have another point of view on Japan’s global contribution given that the telemedicine system is native to Japan. I think a strong point of Japanese medicine lies in its creative, artisanal aspect, affected not only by knowledge but also by culture. This point has not been brought to bear as yet, but digital technology such as digital therapeutics will be able to empower the field of telemedicine and export it from Japan to the world.
(Sakano)
There are no ophthalmologists in Rwanda and Kenya has only 60 cardiovascular doctors. I discussed with the people in these countries that there is no choice but to create a new country-wide medical system through distance education and telemedicine. Japan is expected to play its part in this context, and I would like to develop telemedicine education through various collaborations.
(Kobayashi)
We would like to create an environment that increases the number of doctors who can perform robotic surgery in developing countries and remote areas by connecting remote surgery training globally.
(Asonuma)
Medical systems such as free access offer world-class medical care in Japan. However, these systems require the increase of management entities. Also, many backward hospitals still do not gather medical data, which causes various problems. In fact, few non-medical staff can support medical care in Japan, and the burden on doctors appears to be too heavy. To address issues in all these areas, it will be necessary to have considerable discussions.
(Sonno)
Emergency medical care in Japan is excellent but supported mainly by individual efforts and culture. We are considering how to export medical care overseas, including education, but there are no answers as yet. In Japan, it will be necessary to promote the transfer of authority to younger people. Young people with a business sense in DX will be able to beat the older generation.
(Yahagi)
A mechanism to support medical care based on technology while incorporating tacit clinical knowledge is indispensable. All included data must be vital and specifically used to treat and save patients through the universal health insurance system which only exists in Japan. However, today’s universal health insurance is not a long-term reality, so if we can build something for the next-generation insurance system that does not involve risks, then, as pointed out earlier, every country will want it.
Closing Remarks
Kiyoshi Kurokawa, Professor Emeritus,
The University of Tokyo and National Graduate Institute for Policy Studies,
and Distinguished Professor of Tokai University

Send the Next Generation Off
Now that we have a digital society, we have to think about what each person can do from a worldwide perspective.
The most important thing for young people is to grow up and assert themselves. Japan is the longest-lived society, with women accounting for the highest proportion of the elderly. Furthermore, it is a society with a declining birth rate. Only women can give birth to children, but do men fully appreciate that fact? Why would women want to give birth to two or three children in our society? There are only men present on this panel, right? You may not find this kind of situation in places like the United States where the present discussion might be regarded as an “older men’s” gathering.
Generally, overseas graduates from universities and graduate schools, as well as postdocs must leave their schools and hospitals upon graduation. This process helps to spread the reputation of the disciple’s professor. Since Japanese people tend to stay in the same place instead of going somewhere else, it is difficult for their superiors’ reputation to spread through society. We have to change this issue.
This situation will not change by trying to involve government offices. So how can we take a step forward? The answer is by sending the next generation off to stand on its own feet. Then we will earn the trust of society. Trust is not easy to earn without experience, so sending students off in the spirit that they need not come back is essential. In the global era, I want the younger generation to go out and foster a healthy patriotism away from their alma mater in order to contribute to improving Japan from an objective perspective.
(written by Hitomi Sano , photo by Shun Arima)
 Contact us
Contact us